Why ApoB and Lipoprotein(a) Can Change the Entire Trajectory of Your Life
The Cholesterol Myth That Keeps People Sick
For decades, we were taught a simple story:
“If your LDL cholesterol is normal, your heart is safe.”
That story is wrong.
Every week, I see patients who:
Exercise regularly
Eat reasonably well
Have “acceptable” LDL cholesterol
…and still develop coronary plaque, heart attacks, or strokes.
The reason is simple: LDL cholesterol is not the same thing as LDL particles.
And particles are what damage arteries.
That’s where ApoB and Lipoprotein(a) come in.
The Cholesterol Myth That Keeps People Sick
For decades, we were taught a simple story:
“If your LDL cholesterol is normal, your heart is safe.”
That story is wrong.
Every week, I see patients who:
Exercise regularly
Eat reasonably well
Have “acceptable” LDL cholesterol
…and still develop coronary plaque, heart attacks, or strokes.
The reason is simple: LDL cholesterol is not the same thing as LDL particles.
And particles are what damage arteries.
That’s where ApoB and Lipoprotein(a) come in.
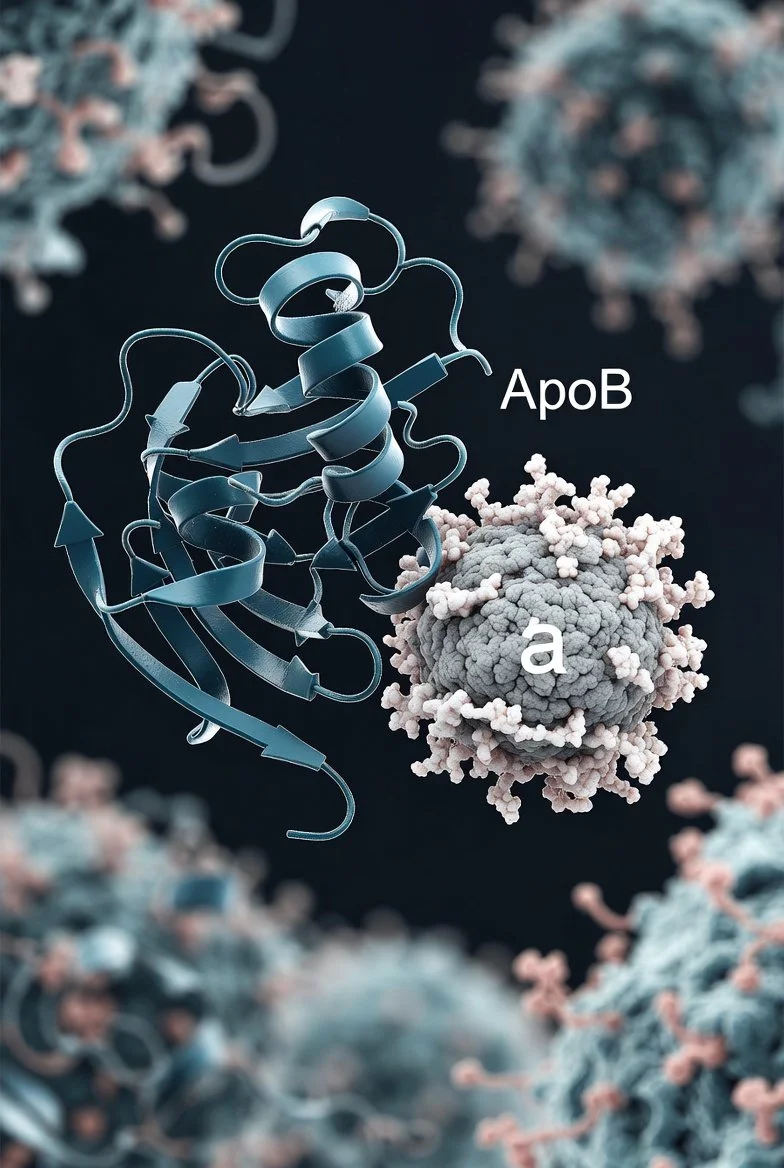
ApoB: The Particle Count That Actually Matters
Apolipoprotein B (ApoB) is a protein found on every atherogenic (artery-damaging) particle:
LDL
VLDL
IDL
Remnant particles
One particle = one ApoB molecule.
So ApoB tells us the true number of cholesterol-carrying particles circulating in your blood.
Why This Changes Everything
Two people can have the same LDL cholesterol:
Person A: Few large particles → lower risk
Person B: Many small particles → much higher risk
Standard cholesterol panels cannot reliably tell the difference.
ApoB can.
Torre Prime Longevity Insight
In Medicine 3.0, we care about lifetime arterial exposure, not whether today’s labs look “okay.”
Lower ApoB = fewer arterial injuries = more decades of healthy life.
Lipoprotein(a): The Genetic Risk Most Doctors Never Measure
Lipoprotein(a)—often written as Lp(a)—is a genetically inherited LDL-like particle with an added protein called apolipoprotein(a).
This extra protein makes Lp(a):
More inflammatory
More adhesive to artery walls
More resistant to breakdown
The Uncomfortable Truth
Your diet barely affects Lp(a)
Exercise barely affects Lp(a)
Many statins barely affect Lp(a)
You are largely born with it.
And if it’s high, your cardiovascular risk is significantly elevated, even with perfect lifestyle habits.
Many heart attacks in fit, lean, active people are explained by undiagnosed high Lp(a).
Why These Two Markers Are Life-Changing Together
ApoB tells us how many artery-damaging particles you have and determines cumulative vascular injury.
Lp(a) is a genetic “accelerant” of plaque and clotting and explains early or unexpected heart disease.
Together, they reveal:
Why plaque forms early
Why family history matters
Why “normal cholesterol” can still be dangerous
This is risk mapping, not guesswork.
What Torre Prime Does Differently
At Torre Prime, ApoB and Lp(a) are Sentinel-level markers—not optional add-ons.
We use them to:
Reframe cardiovascular risk decades earlier
Personalize lipid strategies beyond LDL
Decide how aggressive prevention should be
Integrate imaging (CAC, CTA) intelligently
Align lifestyle, medication, and training with your biology
This is not about fear.
It’s about clarity and control.
What Should Your Numbers Be?
General longevity-oriented targets (individualized per person):
ApoB:
Optimal: ~60 mg/dL or lower
High-risk individuals: often lower
Lipoprotein(a):
Ideally: as low as possible
Elevated risk often begins above ~75–100 nmol/L
These are not one-size-fits-all, and numbers only matter in context—your age, family history, imaging, and goals.
The Bigger Picture: Time Is the Real Risk Factor
Atherosclerosis is not sudden.
It’s:
Quiet
Slow
Cumulative
ApoB tells us how fast the damage accumulates.
Lp(a) tells us whether the process is accelerated.
When you know these early, you gain something priceless:
Time.
Time to intervene.
Time to course-correct.
Time to protect decades of strength, cognition, and independence.
The Torre Prime Philosophy
We don’t wait for symptoms.
We don’t chase emergencies.
We don’t accept “normal” when better is possible.
ApoB and Lipoprotein(a) aren’t just lab tests.
They’re maps of your future.
And maps are only powerful when you use them.
Why Your Bloodwork Might Be “Normal” — But You Still Feel Off
Why Your Bloodwork Might Be “Normal” — But You Still Feel Off
Most people are told the same thing after routine lab work:
“Everything looks normal.”
And yet they still feel off.
Low energy. Brain fog. Poor sleep. Weight that won’t budge. Mood changes. Diminished libido. Slower recovery. A vague sense that something isn’t right — even though nothing is “wrong enough” to diagnose.
At Torre Prime, we see this every week.
The problem isn’t that you’re imagining symptoms.
The problem is that “normal” bloodwork was never designed to optimize human performance or longevity.
It was designed to detect late-stage disease.
Most people are told the same thing after routine lab work:
“Everything looks normal.”
And yet they still feel off.
Low energy. Brain fog. Poor sleep. Weight that won’t budge. Mood changes. Diminished libido. Slower recovery. A vague sense that something isn’t right — even though nothing is “wrong enough” to diagnose.
At Torre Prime, we see this every week.
The problem isn’t that you’re imagining symptoms.
The problem is that “normal” bloodwork was never designed to optimize human performance or longevity.
It was designed to detect late-stage disease.
“Normal” Is a Statistical Concept — Not a Health Goal
Most lab reference ranges are created by sampling the general population.
That population includes:
Sedentary individuals
Insulin resistance
Poor sleep
Chronic inflammation
Early cardiometabolic disease
So when your results come back “within range,” what that really means is:
You’re statistically similar to the average person — not biologically optimized.
Longevity medicine asks a different question:
Are your labs supporting long-term cardiovascular health, brain health, metabolic resilience, and vitality — or quietly eroding them?
The Gap Between Disease Detection and Longevity Optimization
Traditional medicine focuses on thresholds:
Diabetes vs. no diabetes
Heart disease vs. no heart disease
Kidney failure vs. normal kidneys
Longevity medicine focuses on trajectories:
Where is your metabolism heading?
How much vascular damage is accumulating quietly?
Are your mitochondria efficient or stressed?
Are your labs drifting toward disease — years before symptoms appear?
This is where people feel “off” long before anything flags red.
ApoB: The Number Most Panels Don’t Emphasize (But Should)
One of the biggest blind spots in standard bloodwork is Apolipoprotein B (apoB).
ApoB represents the number of atherogenic particles circulating in your bloodstream — the particles that actually enter artery walls and drive plaque formation.
Why apoB matters more than LDL cholesterol
LDL-C measures cholesterol content
ApoB measures particle count
More particles = more opportunities for arterial damage
You can have:
“Normal” LDL
“Normal” total cholesterol
Elevated apoB and rising cardiovascular risk
From a longevity perspective, apoB is one of the strongest modifiable predictors of heart disease, which remains the leading cause of death worldwide.
At Torre Prime, we don’t ask:
“Is this lab technically normal?”
We ask:
“Is this lab aligned with decades of vascular health?”
Sugar Metabolism: You Can Be “Normal” and Still Insulin Resistant
Fasting glucose and A1c often appear normal — even as metabolic dysfunction is developing underneath.
This happens because:
Your pancreas can compensate for years
Insulin levels rise before glucose does
Blood sugar stays “normal” at the cost of metabolic strain
Early insulin resistance contributes to:
Fatigue
Brain fog
Inflammation
Weight gain
Hormonal disruption
Cardiovascular risk
From a longevity lens, we care deeply about:
Insulin sensitivity
Metabolic flexibility
How efficiently your cells use fuel
Because poor sugar handling ages every organ system simultaneously.
Cholesterol Metabolism Is More Than “Good” and “Bad”
The outdated HDL/LDL framing misses critical nuance.
Longevity medicine looks at:
Particle number and size
ApoB burden
Triglyceride dynamics
Insulin-cholesterol interaction
Inflammation and oxidative stress
Why?
Because cholesterol transport is tightly linked to:
Liver health
Muscle insulin sensitivity
Mitochondrial energy production
Hormone synthesis
When metabolism is stressed, cholesterol becomes a signal of dysfunction, not just a cardiovascular metric.
Why You Feel Off Before Labs Turn Red
Symptoms often precede diagnoses by years or decades.
You might feel:
Tired despite “normal” labs
Mentally foggy despite “normal” labs
Less resilient, less driven, less sharp
That’s because:
Your biology is adapting — not thriving
Compensation is occurring quietly
Systems are strained, not broken
Longevity medicine exists in this gray zone — before damage becomes irreversible.
The Torre Prime Approach: Data Into Direction
At Torre Prime, we don’t chase diagnoses.
We map risk.
We look at:
Cardiometabolic load
ApoB-driven vascular risk
Sugar and lipid metabolism together
Energy systems, not isolated numbers
Then we translate data into:
Training strategies
Nutrition strategies
Sleep optimization
Recovery protocols
Targeted interventions
This is Medicine 3.0 — proactive, preventive, personalized.
The Bottom Line
If your labs are “normal” but you feel off, that doesn’t mean nothing is wrong.
It means:
The right questions haven’t been asked
The right markers haven’t been interpreted
The right time horizon hasn’t been considered
Longevity isn’t about avoiding disease this year.
It’s about protecting the next 20, 30, or 40 years of your life — while feeling strong, clear, and alive along the way.
Why Do I Wake Up in the Middle of the Night?
Why Do I Wake Up in the Middle of the Night?
Understanding 2–4 AM Cortisol Spikes, Stress Physiology & What to Do About It
Waking up in the middle of the night is common—but not normal. Learn why cortisol spikes, blood sugar swings, stress, and hormones trigger 2–4 AM awakenings, and when to seek a physician’s evaluation. Torre Prime explains the science and next steps.
Gabriel Felsen
Understanding 2–4 AM Cortisol Spikes, Stress Physiology & What to Do About It
Waking up in the middle of the night is one of the most common sleep complaints I hear at Torre Prime—especially from people who eat well, exercise, and still can’t stay asleep.
If you find yourself wide awake at 2, 3, or 4 AM, heart a little faster than you’d expect, mind suddenly alert, this article is for you.
And the key player is often cortisol.
Your Body’s Nighttime Cortisol Curve: What’s Supposed to Happen
Cortisol follows a natural 24-hour rhythm:
Lowest around midnight
Begins rising around 2–3 AM
Peaks around 7–9 AM to help you wake naturally
Gradually falls throughout the day
When everything is working smoothly, you sleep through the small early-morning rise without noticing.
But certain factors can cause an exaggerated cortisol spike, and that’s when people wake up—alert, restless, sometimes anxious.
Why Cortisol Spikes Wake You Up
You may be experiencing a nighttime cortisol surge if your awakening feels like:
Sudden alertness rather than a gentle stir
Heart rate a little elevated
Busy thoughts or problem-solving mind
Difficulty falling back asleep despite feeling “tired”
Common reasons your cortisol rhythm can misfire:
1. Blood Sugar Drops Overnight
If you eat a high-carbohydrate or late dinner, your blood sugar can swing low at night.
The body responds by releasing cortisol (a glucose-releasing hormone), which can wake you up.
2. Chronic Stress & Sympathetic Overdrive
Unresolved stress shifts your nervous system toward “fight or flight,” which increases nighttime awakenings.
Conditions like overtraining, emotional burnout, and nighttime rumination amplify this.
3. Alcohol
Even small amounts disrupt REM sleep, increase nighttime heart rate, and cause early-morning cortisol spikes.
4. Hormonal Changes
Perimenopause, low testosterone, thyroid imbalance, and growth hormone decline all affect nighttime recovery and cortisol balance.
5. Sleep Fragmentation from Poor Downstate Reserves
As Dr. Sara Mednick explains in Power of the Downstate, your body needs deep daytime restoration (parasympathetic recovery) to support consolidated sleep. Without this, you’re more likely to wake up in the early morning hours.
6. Hidden Sleep Disorders
Sleep apnea and upper-airway resistance can activate the sympathetic nervous system and fragment sleep even in lean, athletic, or “normal-sleeping” people.
A Few Things You Can Try Tonight
These strategies are safe, gentle, and appropriate for most people—but the root cause often needs medical evaluation.
Stabilize Blood Sugar Before Bed
Try:
A small protein-rich snack before bed (e.g., cottage cheese, Greek yogurt, a handful of nuts)
Avoiding high-sugar desserts within 2–3 hours of sleep
For many Torre Prime patients, this alone reduces early-night and early-morning wakeups.
Support a Calmer Nighttime Nervous System
Simple, evidence-aligned practices:
5–10 minutes of slow breathing before bed
A warm shower
Gentle stretching
Ending screens 30–60 minutes before sleep
These increase parasympathetic tone and smooth the cortisol curve.
Helpful Supplements (Generally Safe, But Not Always Enough)
These can be supportive but are not substitutes for medical evaluation:
Magnesium glycinate (100–200 mg) to help relax the nervous system
L-theanine (100–200 mg) for calming racing thoughts
Glycine (3 g) to gently lower core body temperature
Ashwagandha for chronic stress regulation
Phosphatidylserine for elevated nighttime cortisol (needs professional guidance)
Always check with a physician if you take medications, have thyroid disease, are pregnant, or have autoimmune conditions.
When Middle-of-the-Night Waking Is a Sign of Something Else
At Torre Prime, we evaluate:
Cortisol rhythm (salivary or urine testing)
Heart-rate variability trends
Blood sugar dysregulation
Thyroid function
Testosterone and estradiol
Sleep apnea risk
Alcohol patterns, caffeine timing, and nighttime light exposure
Overtraining vs. under-recovery patterns
Nervous system imbalance
Sleep is one of the strongest levers for long-term cognitive and metabolic health. Frequent awakenings—even if short—can impair glucose control, cognition, emotional resilience, and cardiovascular risk.
When It's Time to Get a Physician Involved
You should seek a medical evaluation if:
You wake up in the middle of the night more than 3 times a week
The awakenings feel stressful, sudden, or heart-related
You feel unrefreshed even after 8+ hours in bed
You rely on supplements or alcohol to fall back asleep
You snore, wake with a dry mouth, or suspect fragmented breathing
You’re in your 40s–60s and your sleep has changed without explanation
You feel exhausted during the day despite “normal” sleep duration
A personalized plan is almost always more effective than self-treating.
The Torre Prime Approach
At Torre Prime, your sleep evaluation includes:
Mapping nighttime awakenings to physiologic patterns
Oura/Whoop HRV and temperature trend interpretation
Assessing cortisol rhythm, metabolic signals, and recovery debt
Looking at nutrient status, hormones, and cardiometabolic drivers
Designing a structured plan using Medicine 3.0 principles
Creating a personalized Downstate protocol to stabilize nighttime recovery
Follow-up accountability so changes actually happen
Most patients experience improvement within 2–4 weeks once the underlying drivers are identified.
The Bottom Line
Waking up in the middle of the night is common, but not normal.
It usually means your body is trying to tell you something—about stress, metabolism, recovery, hormones, or sleep physiology.
You can try the simple strategies above, but persistent awakenings usually need physician input to uncover the real cause and build a targeted plan.
If your nighttime wakeups have become a pattern, Torre Prime can help you understand why—and guide you toward deeper, more stable, more restorative sleep.